A new study led by the U.S. Military HIV Research Program (MHRP) has shown that active HIV reservoir that persists even during suppressive antiretroviral therapy (ART) is correlated with increased HIV-specific CD8+ T cell immune response, but prevents them from becoming fully functional. This suggests that strategies targeting the active HIV reservoir hold promise for functional “cure” therapies to bring about long-term HIV remission. Findings were published this week in Cell Host & Microbe.
HIV-specific CD8+ T cells are white blood cells that kill cells infected with HIV. Previous studies have found that before ART initiation, HIV-specific CD8+ T cells are dysfunctional, and ART initiation only partially restores CD8+ T cell function. CD8+ T cells with high functionality have been considered key to achieving HIV control in elite controllers.
In the recent study, researchers analyzed the associations between the magnitude and functionality of HIV-specific CD8+T cells and the active HIV reservoir on ART in people treated in acute and chronic infection. They compared samples from 48 people with HIV from MHRP’s RV254 acute infection cohort who initiated ART early, and 18 participants who initiated ART during chronic HIV infection from the RV304 study, all conducted in Bangkok.
They found that a larger active reservoir while on therapy elicited a greater CD8+ T cell response, but a smaller active reservoir while on therapy was associated with greater CD8+ T cell functionality.
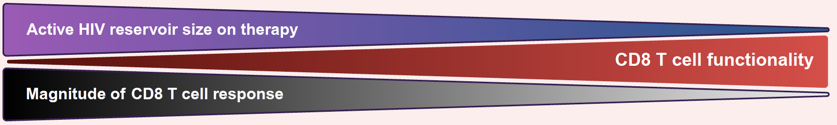
This has implications for strategies for a functional HIV “cure,” or long-term remission of HIV without ART. “Interventions aimed at decreasing active HIV on ART might encourage development of differentiated of functional HIV-specific CD8+ T cells that are able to mount rapid recall immune responses and control rebounding virus after ART is stopped,” said Dr. Lydie Trautmann, MHRP’s Director of Translational Research.
